Tracking New Jersey’s Opioid Settlement Funds: Year Three

By Nikki Tierney, JD, LPC, LCADC, CPRS
NCAAR Policy Analyst
December 2025
“If nothing changes, nothing changes.” — Unknown
As we enter our third year of tracking how New Jersey and its subdivisions are spending—or failing to spend—the opioid settlement dollars entrusted to them, we are sharpening our focus. In past years, we have monitored the state, municipalities, and counties alike. This year, our attention is on the counties–because while the Murphy administration has begun moving state dollars aggressively (another $130.7 million committed in September 2025 alone for harm reduction and family support), far too many counties are still sitting on millions while residents struggle.1 Yet through all of this, one fact remains unmistakable: opioid use disorder is highly treatable. Lives are saved when evidence-based prevention, treatment, harm reduction, and recovery supports are funded and delivered, not delayed.
This year, our report goes beyond tracking dollars. We pair the latest county-level data with research-supported recommendations designed to help local governments meet their fiduciary responsibilities. Our goal is simple: ensure that money intended to save lives is finally used for that exact purpose.
New Jersey is finally seeing the results we fought for. Provisional data show overdose deaths dropping sharply—from a peak of 3,171 in 2022 to 2,816 in 2023, an estimated 1,803 in 2024, and on pace for even fewer this year— approximately 1,200-1,400 in 2025 based on provisional mid-year declines.2 Harm reduction works. Treatment works. Naloxone works. Recovery support works. But the state’s progress only underscores some of the stagnation at the county level.
Please note: Although we focus on just one of the ways counties can begin to mobilize the life-saving funding at their disposal, there are multiple evidence-based strategies that promote recovery and community resilience. The Opioid Settlement Advisory Group (OSAG), of which NCAAR is a founding member, is a peer-driven initiative that brings together individuals with lived experience, stakeholder organizations, family members, and allies. OSAG’s NJ Opioid Settlement Roadmap presents evidence-based ways opioid settlement funds can be used to make a significant difference in the lives of those affected by the opioid crisis, including investments in housing, transportation, family support, grassroots initiatives, public health interventions, and employment support.
Spending Patterns: What the Numbers Reveal
Before diving into recommendations, it’s important to ask a simple but critical question: how much of New Jersey’s opioid settlement funding has been spent? The table below summarizes county-level allocations, remaining balances, and percentages spent based on the most recent public reports submitted to the state.3 How much of New Jersey’s opioid settlement money has reached the people who need it? The answer, three years in, is disheartening.
Of the more than $109 million distributed to counties since 2022, most remains unspent. Fifteen of New Jersey’s twenty-one counties have used less than one-third of their allocations, and seven have spent 10% or less. Four counties even report negative spending, suggesting issues in how funds are being tracked or reported.
As a result, tens of millions of dollars intended for treatment, harm reduction, and community support remain idle. When compared with local need, the gaps become even more pronounced:
- Essex County, which accounts for 10% of all treatment admissions, has spent only 3.1% of its available funds.
- Atlantic and Camden Counties (each representing 9% of admissions) have spent 22.6% and 37.7%, respectively.
- Hudson County, responsible for 5% of statewide treatment admissions, reports 0% spending.
- Bergen County is holding $8.6 million in unspent funds (95.6% of its allocation) while serving just 4% of the state’s treatment population.
Meanwhile, tiny Sussex County (1% of admissions) has managed to spend 46.6%. Action is clearly possible when leaders treat this like the emergency it is. This data illustrates a troubling disconnect: settlement funds are not being allocated in proportion to need, nor at a pace that reflects the urgency of the crisis. Entering the third year of this analysis, the consequences of inaction are stark, while opportunities to save lives have never been clearer. All told, counties hold approximately $70 million unspent— funds that could support services for tens of thousands of people if deployed now.
| New Jersey County | Total Received Since 2022 | Unspent/Remaining Funds | Percentage Spent | Total Residents Treated (2023) | Percentage of Statewide Treatment Admissions |
|---|---|---|---|---|---|
|
|
|||||
| Atlantic | $5,061,802.06 | $3,916,798.41 | 22.6% | 7,213 | 9% |
| Bergen | $8,984,163.48 | $8,588,581.76 | 4.4% | 3,083 | 4% |
| Burlington | $8,559,418.49 | $5,818,662.81 | 32.0% | 3,963 | 5% |
| Camden | $12,493,217.93 | $7,787,499.77 | 32.0% | 3,963 | 9% |
| Cape May | $2,248,171.54 | $2,604,966.56 | -15.9% | 2,096 | 3% |
| Cumberland | $1,726,521.30 | $1,709,022.20 | 1.0% | 3,172 | 4% |
| Essex | $3,333,703.06 | $3,231,754.84 | 3.1% | 7,642 | 10% |
| Gloucester | $8,231,359.00 | $7,587,999.00 | 7.8% | 4,033 | 5% |
| Hudson | $1,639,073.79 | $1,638,711.45 | 0.0% | 3,572 | 5% |
| Hunterdon | $1,815,411.05 | $1,784,813.69 | 1.7% | 691 | 1% |
| Mercer | $2,219,630.51 | $1,935,513.64 | 12.8% | 3,745 | 5% |
| Middlesex | $3,384,737.25 | $3,477,720.73 | -2.8% | 5,678 | 7% |
| Monmouth | $7,776,400.28 | $4,473,268.98 | 42.5% | 6,094 | 8% |
| Morris | $4,708,294.95 | $3,277,939.28 | 30.4% | 1,723 | 2% |
| Ocean | $8,979,492.70 | $5,464,668.20 | 39.1% | 6,440 | 8 % |
| Passaic | $3,612,431.59 | $2,202,120.04 | 39.0 % | 4,122 | 5 % |
| Salem | $1,645,992.01 | $1,517,927.87 | 7.8 % | 927 | 1 % |
| Somerset | $1,507,600.47 | $1,611,961.39 | -6.9 % | 1,554 | 2 % |
| Sussex | $2,318,762.53 | $1,237,423.42 | 46.6 % | 993 | 1 % |
| Union | $3,301,777.94 | $2,233,695.31 | 32.4 % | 3,440 | 4 % |
| Warren | $1,810,419.95 | $2,106,961.42 | -16.4 % | 1,023 | 1 % |
| TOTAL | 78,416 | 100% |
The data in this table comes from New Jersey Attorney General’s Office. (2025). County Opioid Abatement Reports, Q2 2025 (covering expenditures from January 2022–June 2025). Available at: https://www.nj.gov/opioidfunds/important-documents/reports/index.shtml (Individual county PDFs submitted quarterly; aggregated data as of July 2025). And New Jersey Department of Human Services, Division of Mental Health and Addiction Services. (2024). Substance Abuse Overview: 2023 Statewide. https://www.nj.gov/humanservices/dmhas/publications/statistical/Substance%20Abuse%20Overview/2023/Statewide.pdf.
Even communities that have misapplied settlement funds have still managed to spend more than many counties holding tens of millions unused. The New Jersey Office of the State Comptroller (OSC) reported that Irvington misused over $632,000 in opioid settlement funds by hosting two “opioid awareness” concerts in 2023 and 2024, which had little or no focus on health outcomes.4 Acting State Comptroller Kevin Walsh emphasized: “These funds are supposed to be lifelines for communities overwhelmed by the opioid epidemic — not a slush fund to host concerts and throw parties.”5
While spending opioid settlement funds on concerts is clearly a misuse of taxpayer dollars and not the intended evidence-based intervention, it begs a rhetorical question: is some public engagement—even if misdirected—better than leaving the funds completely untouched?
Leaving opioid settlement funds unspent is particularly confusing given that opioid use disorder (OUD) is highly treatable. A robust body of evidence supports medications for opioid use disorder (MOUD)—including methadone, buprenorphine, and naltrexone—which dramatically reduce overdose risk and improve long-term recovery outcomes. Despite their proven effectiveness, these treatments remain vastly underutilized, leaving lives at risk while millions of dollars intended to expand access, prevent harm, and save lives remains inactive.
MOUD Works: Evidence-Based Life-Saving Treatment
Medications for opioid use disorder (MOUD) are among the most effective and powerful tools for saving lives and improving outcomes for people with OUD. A recent multi-state study of nearly 2,000 adults receiving OUD treatment at 62 outpatient facilities across 16 states provides compelling evidence.6 Participants were followed for 18 months, with data collected from self-reported surveys and health records. By the end of the study:
- The proportion of individuals maintaining abstinence increased from 55% to 77%.
- Opioid-related overdoses dropped from 7% to 2%.
- Emergency department visits decreased from 9% to 4%.
- Arrests fell from 15% to 7%.

The study demonstrates that consistent, evidence-based treatment dramatically improves outcomes—not only by reducing opioid use, but also by preventing overdoses, easing hospital burdens, and lowering criminal system involvement.
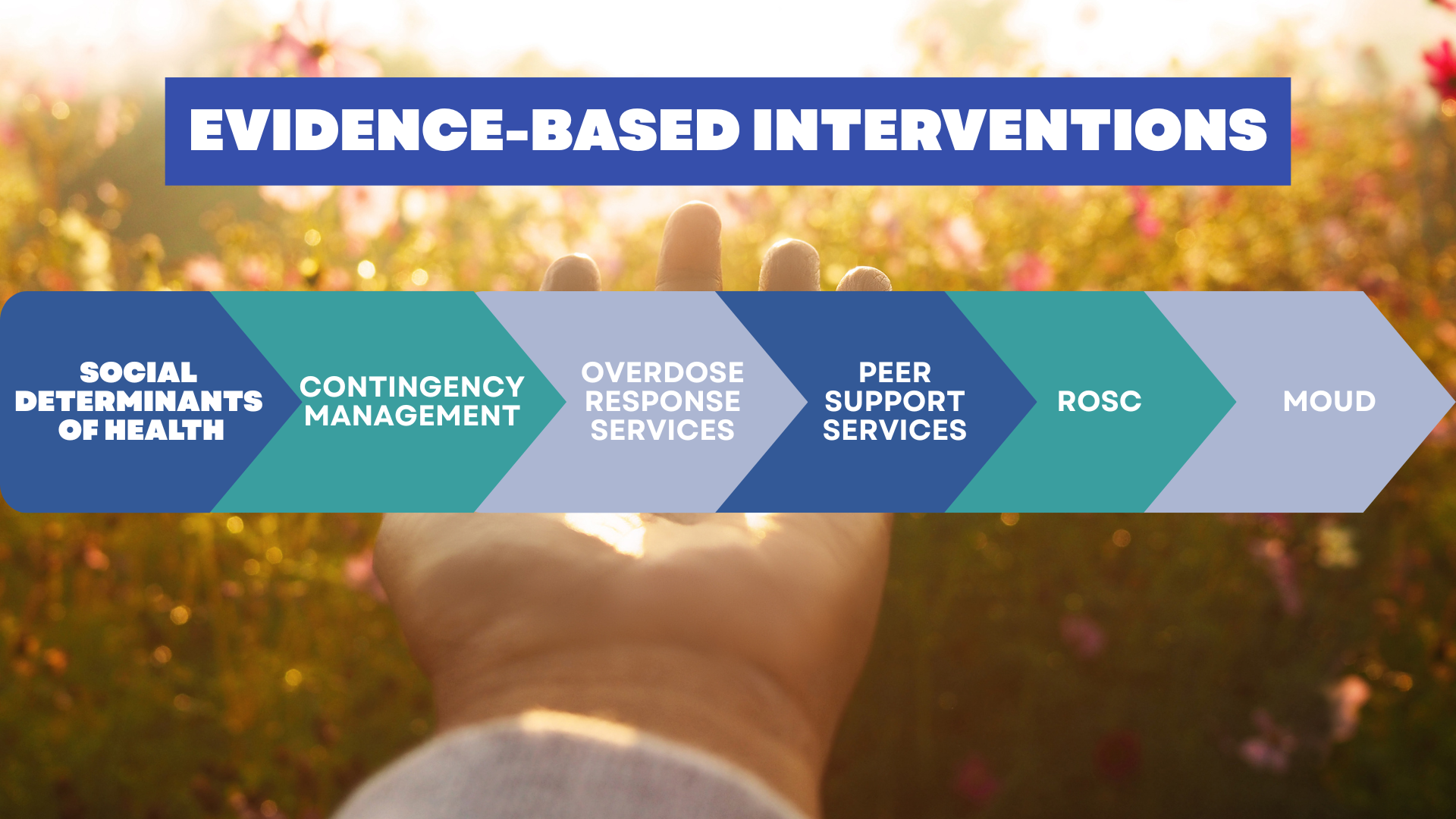
Expanding Evidence-Based Interventions Saves Lives
A recent decision-analytical study modeled the effects of expanding access to MOUD, enhancing treatment retention, and scaling up overdose education and harm reduction services for people with OUD.7 Among over 16 million individuals not currently receiving MOUD and 1.7 million already in treatment, the model projected that combining these interventions could:
- Decrease OUD prevalence by 23%
- Expand MOUD treatment by 137%
- Reduce nonfatal overdoses by 35% and fatal overdoses by 37% (2021–2023)
The study highlights that scaling up evidence-based strategies—particularly those directly reducing overdose risk—can achieve the greatest short-term reductions in fatal overdoses.
Expanding access to MOUD is particularly critical for vulnerable populations, including veterans, people who are incarcerated, and those recently released, who face heightened risk of overdose and mortality. Research on veterans with OUD in the U.S. Veterans Health Administration found that even short-term treatment (<6 months) with methadone or buprenorphine lowers mortality compared with no treatment. Importantly, longer retention in treatment further amplifies these life-saving benefits, even though risks increase during transitions into and out of care.8
 A study published in The New England Journal of Medicine, supported by the NIH, found that providing MOUD to incarcerated individuals substantially improves post-release outcomes.9Among 6,400 individuals with probable OUD incarcerated in seven Massachusetts county jails (Sept 2019–Dec 2020), those who received MOUD were much more likely to stay engaged in treatment six months post-release. They also experienced a 52% lower risk of fatal opioid overdose, a 24% lower risk of nonfatal overdose, a 56% lower risk of death from any cause, and a 12% lower risk of reincarceration compared to those who did not receive MOUD. These results underscore the essential role of providing MOUD in correctional settings to save lives and reduce harm.
A study published in The New England Journal of Medicine, supported by the NIH, found that providing MOUD to incarcerated individuals substantially improves post-release outcomes.9Among 6,400 individuals with probable OUD incarcerated in seven Massachusetts county jails (Sept 2019–Dec 2020), those who received MOUD were much more likely to stay engaged in treatment six months post-release. They also experienced a 52% lower risk of fatal opioid overdose, a 24% lower risk of nonfatal overdose, a 56% lower risk of death from any cause, and a 12% lower risk of reincarceration compared to those who did not receive MOUD. These results underscore the essential role of providing MOUD in correctional settings to save lives and reduce harm.
Finally, a 2024 study published in the Journal of Substance Use and Addiction Treatment evaluated a 2019 Massachusetts law requiring county jails to provide all three FDA-approved MOUD medications: methadone, buprenorphine, and naltrexone. Seven of the thirteen jails implemented pilot programs, creating an opportunity to assess the public health impact of jail-based MOUD. Among 375 individuals treated between January 2019 and December 2020, jail-based MOUD reduced overdose deaths immediately after release and achieved high retention for filling the first buprenorphine prescription post-release. The study underscores that providing MOUD in all correctional facilities is essential to maximize life-saving benefits.
These are not theoretical gains. These are thousands of mothers, fathers, sons, and daughters whose lives could change with access to the proper resources. In New Jersey, counties are sitting on tens of millions of dollars explicitly intended to expand MOUD, naloxone distribution, housing, and peer support—while drug-related deaths, though finally falling, remain far higher than they should be. Every day a county delays is another day someone is waiting for the services we already know saves lives.
Policy Consensus: Every Major Authority Says the Same Thing — Spend the Money on MOUD Now

This is no longer a debate. Every credible authority in America has declared medications for opioid use disorder the gold standard of care:
- The Joint Commission (August 2024) now requires all accredited behavioral health organizations to safely initiate and maintain MOUD — making it an official standard of care, not an option.10 This policy endorsement confirms that MOUD is not only effective but also an established standard of care.
- The American Medical Association, American Society of Addiction Medicine, CDC, SAMHSA, NIDA, and the National Academy of Medicine all classify MOUD as first-line, life-saving treatment.
- The U.S. Surgeon General (2018, reaffirmed 2024) called denying MOUD “equivalent to denying insulin to someone with diabetes.”
- The National Council for Mental Wellbeing and the Legal Action Center list expanding MOUD as the #1 approved use of opioid settlement dollars nationwide.
Recent data from the New Jersey Department of Health offers both hope and a sober reminder of the challenges ahead. According to the 2025 Strategic Plan from the NJ Opioid Recovery and Remediation Advisory Council, the state recorded 2,816 overdose deaths in 2023, marking an 11% decrease from 2022.11 Meanwhile, all 21 counties now have at least one authorized Harm Reduction Center providing access to buprenorphine, naloxone, and other essential services. Still, despite these gains, access remains far from universal. A recent study shows that while prescriptions for opioid use disorder at community health centers in New Jersey have more than doubled over the past six years, less than 25% of patients with OUD at these clinics received MOUD in 2023.
New Jersey’s own leadership agrees on the path forward. Governor Murphy’s Opioid Recovery and Remediation Advisory Council explicitly ranks MOUD expansion, low-barrier buprenorphine access, and harm-reduction services as top priorities for settlement spending. The state’s own Exhibit B (approved strategies from the 2022 Memorandum of Agreement) puts “initiating or expanding MOUD in clinics, jails, and re-entry programs” at the very top of the list, alongside naloxone distribution and recovery supports. This playbook—drawn from national settlements and tailored for NJ—mandates evidence-based spending, with over $130 million already allocated statewide for these interventions.12
Despite broad agreement among public health experts and ample settlement dollars available, why haven’t counties moved funding to interventions proven to yield such a positive impact? MOUD reduces overdose risk by 50% and mortality by up to 38%, but only one in five eligible New Jerseyans has access.13 To turn this around, we urge counties to: (1) Allocate funds to MOUD expansion; (2) Partner with Harm Reduction Centers for low-barrier access; (3) Report quarterly on outcomes, not just dollars. Aligning spending with evidence is no longer optional, but critical to ensure the funds meant to remediate the harms caused by the opioid epidemic actually reach the people it has harmed.
- [↩]New Jersey Department of Human Services, “Governor Murphy Announces $130.7 Million in Opioid Settlement Funding,” Sept 17, 2025 https://www.nj.gov/humanservices/news/pressreleases/2025/approved/20250917.shtml
- [↩]NJ DOH Opioid Dashboard (provisional 2022–2025 data); NJ Opioid Recovery & Remediation Advisory Council 2025 Strategic Plan.https://www.nj.gov/health/news/2025/approved/20250326a.shtml
- [↩]New Jersey Opioid Settlement County Expenditure Reports (Q2 2025), nj.gov/opioidfunds.
- [↩]New Jersey Office of the State Comptroller, “An Investigation of Irvington’s Mismanagement of Opioid Settlement Funds,” July 8 2025 (https://www.nj.gov/comptroller/library/reports/IRV/2025_07_08_irvington_finalized_report.pdf
- [↩]“Irvington Used Opioid Settlement Money as ‘Slush Fund’ for Concerts, Watchdog Says.” The New Jersey Monitor, July 8, 2025. https://www.njmonitor.com/irvington-opioid-concerts
- [↩]Dever, J. A., Hertz, M. F., Dunlap, L. J., Richardson, J. S., Wolicki, S. B., Biggers, B. B., Edlund, J., Bohm, M. K., Turcios, D., Jiang, X., Zhou, H., Evans, M. E., & Guy, G. P., Jr (2024). The Medications for Opioid Use Disorder Study: Methods and Initial Outcomes From an 18-Month Study of Patients in Treatment for Opioid Use Disorder. Public health reports (Washington, D.C. : 1974), 139(4), 484–493. https://doi.org/10.1177/00333549231222479
- [↩]Nataraj N, Rikard SM, Zhang K, et al. Public Health Interventions and Overdose-Related Outcomes Among Persons With Opioid Use Disorder. JAMA Netw Open. 2024;7(4):e244617. doi:10.1001/jamanetworkopen.2024.4617
- [↩]Ching, J. H., Owens, D. K., Trafton, J. A., Goldhaber-Fiebert, J. D., & Salomon, J. A. (2021). Impact of treatment duration on mortality among Veterans with opioid use disorder in the United States Veterans Health Administration. Addiction (Abingdon, England), 116(12), 3494–3503. https://doi.org/10.1111/add.15574
- [↩]PD Friedmann, et al. Medications for Opioid Use Disorder in County Jails: Outcomes After Release. New England Journal of Medicine. DOI: 10.1056/NEJMsa2415987 (2025).
- [↩]The Joint Commission R3 Report #43 (Aug 2024); AMA/ASAM/CDC/SAMHSA/NIDA statements. https://www.jointcommission.org/en-us/standards/r3-report/r3-report-43
- [↩]2025 Strategic Plan, NJ Opioid Recovery & Remediation Advisory Council.https://nj.gov/opioidfunds/documents/strategic-plan/2025A%20-%20Full%20Strategic%20Plan.pdf?v=2025-06-11. New Jersey Opioid Settlement Memorandum of Agreement, Exhibit B (2022), nj.gov/opioidfunds
- [↩]NJ DOH Press Release, March 26, 2025 (53rd Harm Reduction Center).https://www.nj.gov/health/news/2025/approved/20250326a.shtml
- [↩]https://www.nj.gov/health/news/2025/approved/20250829a.shtml