A Perfect Storm: Mental Health and Substance Use Disorder Services Under Siege in New Jersey

By Nikki Tierney, JD, LPC, LCADC, CPRS
NCAAR Policy Analyst
October 2025
As demand for mental health and substance use disorder (SUD) services reaches unprecedented levels, both federal and state budgets are facing substantial funding cuts. The proposed federal budget for fiscal year 2026 (FY26) includes significant reductions to the Community Mental Health Services Block Grant and the Substance Use Prevention and Treatment Services Block Grant, which are vital for community-based organizations providing care. New Jersey could be facing a $360 million annual reduction due to proposed decreases in federal funding and provider assessments which would impact healthcare coverage and public health programs. These financial challenges reflect a broader trend of diminishing behavioral health resources, further limiting access for vulnerable populations. The cuts will not only reduce access to direct treatment services but also strip away funding for critical support that helps people meet their basic needs. With significant data and research indicating social determinants of health have a greater impact on health outcomes than clinical care, these reductions threaten to worsen public health and deepen existing health and social inequities in New Jersey.

The Growing Behavioral Health Crisis
According to State of Mental Health in America the 2024 edition:
-
Prevalence of Mental Illness: Approximately 23% of adults experienced a mental illness in the past year, equating to nearly 60 million Americans.
-
Access to Care: Over 28 million adults with mental illness did not receive treatment, highlighting significant gaps in mental health care access
- Substance Use Disorders: 15% of adults had a substance use disorder in the past year, with 93.5% not receiving any form of treatment.
Behind each of these statistics is a real person—an individual with a life worthy of dignity and support, underscoring the urgent need for accessible mental health and substance use services. Even in the currently funded system, engagement and uptake remain alarmingly low and further reductions in access could have devastating consequences. Unfortunately, the federal government has made several recommendations to dismantle the funding that supports the behavioral healthcare system:
-
A 15% reduction in federal funding for Medicaid, which accounts for one-quarter of all U.S. spending on mental health and substance use treatment services
-
Refusal to enforce parity regulations that would ensure insurance plans cover mental health or substance use disorders similarly to other medical conditions
-
The dissolution of the Substance Abuse and Mental Health Services Administration (SAMHSA) and the Health Resources and Services Administration (HRSA) and consolidating them into one Administration for a Healthy America (AHA). This also includes a $1 billion cut to funding for SAMHSA and HRSA programs
-
Eliminating LGBTQ+ crisis services through the 988 Suicide & Crisis Lifeline
- The Executive Order signed on July 25, 2025, titled “Ending Crime and Disorder on American Streets” that clarified support for some overdose prevention services, like naloxone, but denouncing the overarching evidence-based philosophy of harm reduction.

A woman enters the Great Circle drug treatment center in Salem, Ore., on March 8, 2022.(AP Photo/Andrew Selsky, File)
Consequences of Inadequate Care
Research consistently demonstrates that poor access to behavioral health services has ripple effects throughout communities and economies, contributing to worse health outcomes, less stable employment, loss of housing, and increased risk of suicide. On a personal level, individuals experience worsening symptoms, increased risk of crisis, and erosion of hope. At the community and systems level, gaps in healthcare contribute to significant economic costs with higher rates of emergency department visits and hospitalizations, productivity losses, increased disability claims, and higher healthcare expenses.
We have seen the tangible outcomes that result from the absence of accessible care. For example, Oregon’s decriminalization of drugs under Measure 110 initially appeared groundbreaking—but it faltered due to missing key support systems. A state audit revealed that despite plans to redirect cannabis tax revenue toward treatment and harm reduction, increased services and infrastructure were not in place. As a result, overdose deaths increased and only 1% of individuals ticketed for possession sought support via a designated hotline. The initiative’s failure to meet its goals highlights that policy reform without accessible treatment is ineffective at best—and harmful at worst.1 While New Jersey’s cuts are unrelated to drug policy reform, federal funding changes risk producing the same consequences seen when care is unavailable—higher suffering, preventable crises, and lives lost.
Rural regions across the country are experiencing similar consequences driven by lack of access and stigma. In Michigan’s Huron County, overdose deaths surged by 150% in 2023, despite a statewide decline. This alarming increase was attributed to limited local resources and pervasive stigma surrounding addiction.2 Similarly, due in part to lack of access to care, rural regions experience significantly higher suicide rates compared to urban areas, with rates ranging from 18.3 to 20.5 per 100,000, compared to 10.9 to 12.5 per 100,000 in large urban centers.3 These disparities not only affect individuals who lack care but also impose a substantial economic burden—$44 billion annually in lost productivity due to untreated mental illness in rural economies.4
Notably, these funding reductions are compounded by cuts to programs that support basic needs, such as housing, nutrition, and safety. At a time when poverty, inequity, and barriers to protective factors are already at unprecedented levels, slashing these resources further destabilizes those at greatest risk and undermines the wellness of our communities.
Housing Instability and Homelessness
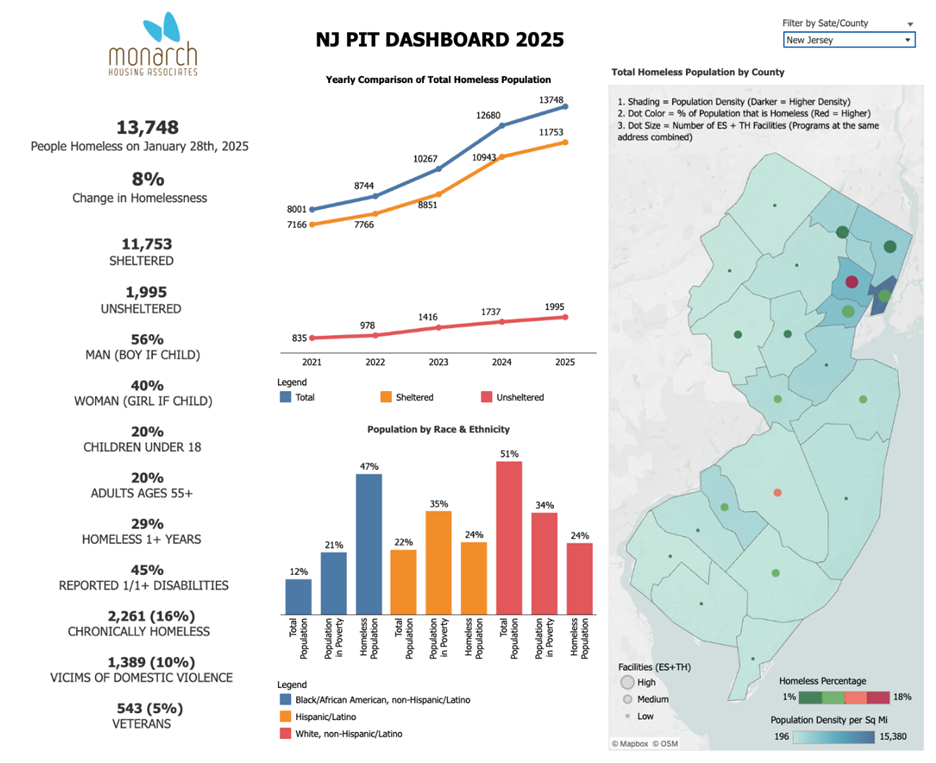
New Jersey has experienced an 8% increase in homelessness, reaching its highest level since 2014. The 2025 Point in Time Count revealed concerning demographic trends. These figures highlight existing structural inequities and how cuts to both direct care and protective resources compound vulnerabilities for marginalized and high-risk populations:
-
Families with children represent approximately one-third of the homeless population.
-
The number of veterans experiencing homelessness has risen by 4.8% from the previous year, totaling 543 individuals.
-
Black residents are disproportionately affected, comprising 47.4% of the homeless population, despite making up only 12% of the state’s overall population.5
New Jersey is also grappling with an escalating affordable housing crisis. The state’s $58.8 billion budget for fiscal year 2026 diverted $125 million from the Affordable Housing Trust Fund, which is the primary public funding source for affordable housing development. This funding cut creates an estimated deficit of nearly 300,000 affordable homes across the state.6 In addition, tens of millions in federal HUD contracts and funding have also been cut. Rep. Rob Menendez (D-8) estimates that roughly 300,000 New Jersey residents rely on federal housing programs, including nearly 40,000 in his district.
Child Care and Cash Assistance Cuts
Funding challenges extend beyond housing. The Child Care Assistance Program (CCAP) faces a $30 million state budget shortfall. As a result:
-
New applications submitted after July 31, 2025, will not be reviewed.
-
Children currently enrolled will continue to receive assistance as long as they remain eligible.
-
Families participating in the program face increased co-payments, with full-time care now costing around 6% of household income.
These limitations restrict access to early childhood care and education, placing additional strain on working families who rely on these critical services to maintain employment and family stability.

Why Cuts to Basic Needs Programs Are So Harmful
 Stable housing, early education, and cash assistance are not “extras,” they are evidence-based public health interventions that prevent crises before they happen. Research consistently shows that housing instability is linked to higher use of emergency departments, higher rates of foster care involvement, and increased school dropout rates. When families lose access to affordable childcare, parents may be forced out of the workforce, placing the family’s ability to meet their basic needs at greater risk.
Stable housing, early education, and cash assistance are not “extras,” they are evidence-based public health interventions that prevent crises before they happen. Research consistently shows that housing instability is linked to higher use of emergency departments, higher rates of foster care involvement, and increased school dropout rates. When families lose access to affordable childcare, parents may be forced out of the workforce, placing the family’s ability to meet their basic needs at greater risk.
Early childhood education, meanwhile, is one of the most effective tools for reducing achievement gaps, improving long-term health, and breaking cycles of generational poverty. These cuts represent more than just budget adjustments; they are disinvestments in prevention and stability. The short-term savings will be outweighed by long-term social and economic costs as recovery becomes even harder for New Jersey’s most vulnerable residents.
The proposed federal cuts to mental health, substance use, and social services represent a significant setback in New Jersey’s laudable and innovative efforts to improve behavioral health care and the health of its residents. Without adequate funding and support, individuals and communities will bear the brunt of these decisions, and the strain extends far beyond healthcare services. The combination of rising demand for behavioral health services and essential support, paired with declining federal funding, creates a “perfect storm” in New Jersey, a state that already has one of the highest costs of living in the country.
It is imperative that policymakers prioritize investment not only in mental health and substance use services but also the essential programs that sustain family and community stability. It is imperative that we, as citizens and community members, voice our deepest hopes for the social system we want to live in—one where health and prosperity are not reserved for the few, but available to everyone. Without these systemic changes, we risk reversing the progress already made and forfeiting future progress, leaving millions without the care and support they desperately need. Currently, the cost of complacency is far too high. In this moment, advocacy has never been more powerful or more essential.
- [↩] Selsky, Andrew. Associated Press. (2023, January 19). Oregon’s drug decriminalization gets poor marks on audit. AP News. https://apnews.com/article/health-oregon-8629d6e62bff151afbbdb3a37c2206ae
- [↩] Snodgrass, K. (2025, June 13). Huron County faces rising overdose rates despite Michigan’s statewide decline. Huron Daily Tribune. https://www.michigansthumb.com/news/article/overdose-deaths-michigan-plummet-rural-counties-20368033.php?utm_source=chatgpt.com
- [↩] Mental Health America. (2025). Rural mental health crisis. Retrieved September 9, 2025, from https://mhanational.org/resources/rural-mental-health-crisis/
- [↩] ZipDo. (2025, May 30). Rural mental health statistics. ZIPDO Education Report 2025. Retrieved September 9, 2025, from https://zipdo.co/rural-mental-health-statistics/?utm_source=chatgpt.com
- [↩] DiFilippo, D. (2025, July 29). Homelessness up again in New Jersey, as federal cuts loom. New Jersey Monitor. https://newjerseymonitor.com/2025/07/29/homelessness-up-again-in-new-jersey-as-federal-cuts-loom/
- [↩] Bansal, P. (2025, July 15). Advocates decry NJ’s budget move as a devastating setback for affordable housing. NJ Urban News. https://njurbannews.com/2025/07/15/advocates-decry-njs-budget-move-as-a-devastating-setback-for-affordable-housing/ Leason, M. (2025, July 3). Advocates say New Jersey budget falls short of affordable housing needs. New Jersey Monitor. https://newjerseymonitor.com/2025/07/03/advocates-say-new-jersey-budget-falls-short-of-affordable-housing-needs/
- [↩]Center on Budget and Policy Priorities. (2023). New Jersey TANF Spending. https://www.cbpp.org/